Patient-Centric Care: Don’t Let EMRs Get in the Way
During his time in the Navy, Salus University president Dr. Michael H. Mittelman, a two-star admiral, had tweaked something in his foot while running and had to go to the Pentagon clinic to see a podiatrist. She examined Dr. Mittelman and as she was doing so, turned away from him and started typing on her laptop.
During his exam, she had taken her concentration off of her patient and turned her attention to the electronic medical records (EMRs) – also known as electronic health records (EHRs) - on her laptop for what Dr. Mittelman thought was an inordinate amount of time.
He relayed his frustrations to the doctor almost immediately, and after the two had a brief exchange, it got Dr. Mittelman thinking. He started talking to other patients to see if they had experienced the same things he had experienced. And for those who had indeed experienced a situation where the doctor was spending more time with the computer than the patient, the consensus was: (1) They don’t really care about me, all they want to do is get the information in and get the next patient in; (2) They didn’t listen to me because the doctor really didn’t look me in the eye. All they were doing was typing on the computer.
“Most lay patients don’t know what the doctor is doing (on the computer) or that they’re required to do this,” said Dr. Mittelman.
 So what began during his Navy career as a concerted effort to practice patient-centric care has carried over into his tenure as Salus president. Prompted by Dr. Mittelman, there is an effort in every clinical facility to make sure student interns take care of the patients first and their EMRs second.
So what began during his Navy career as a concerted effort to practice patient-centric care has carried over into his tenure as Salus president. Prompted by Dr. Mittelman, there is an effort in every clinical facility to make sure student interns take care of the patients first and their EMRs second.
“It’s the de-personalization of care, in my opinion,” he said. “What we’re doing here is not only talking about patient-centric care, but we’re teaching it and we’re forcing the issue. We’re making our students aware of it and we’re reminding them at every step of the way to remember that they’re taking care of the patient. From Day One, we want it to be second nature to our students.”
The introduction of electronic medical records into the doctor’s responsibilities has challenged healthcare providers to find a way to keep the focus on the patients. Since EMRS have been implanted in each of the University’s clinical facilities – The Eye Institute, Pennsylvania Ear Institute and Speech-Language Institute - the collection of data and continuity of care has improved, but care should be taken, according to Dr. Mittelman, not to let the technology infringe on the personal care of the patient.
“Every patient is special, every patient has a story to tell, and as the provider, you need to listen to that story intently and then you act accordingly,” he said. “Our biggest skill should be listening and watching, rather than talking and typing. I feel so strongly about this.”
It’s difficult to achieve that balance, according to Dr. Marie Parisi, associate dean clinical affairs in the University’s Pennsylvania College of Optometry (PCO), which oversees care at The Eye Institute’s three locations.
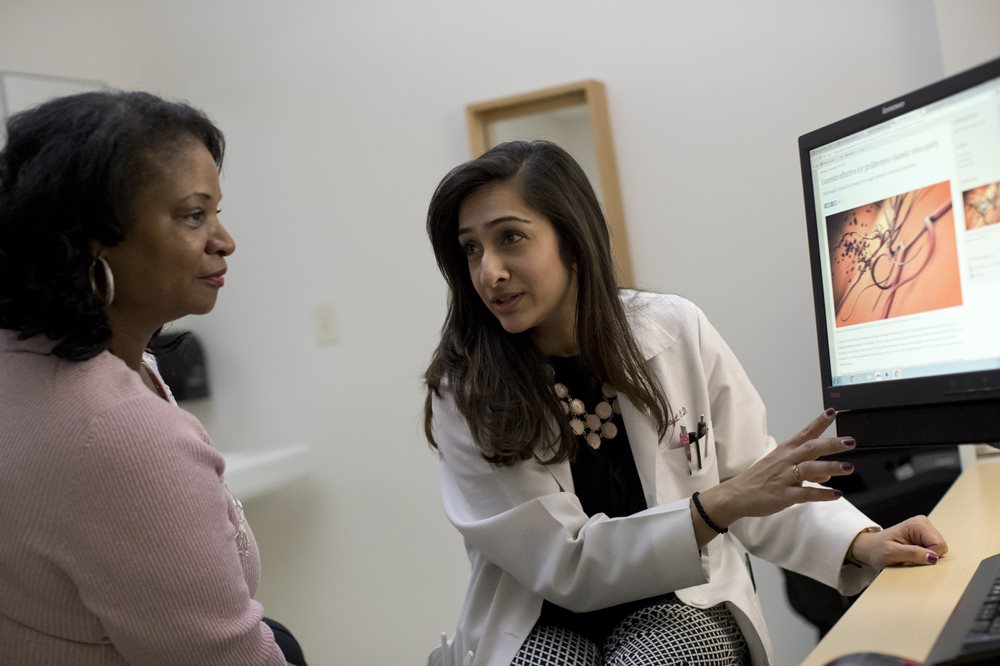 “At The Eye Institute, it’s very individualized based on who the doctor is. We try to have our computers situated to the side, so the screen is facing the provider and the back of it is facing the patient,” said Dr. Parisi. “For an eye exam, there are times when you can’t get by without recording some stuff in the EMR. But our computers (in an exam room) are such that we can kind of look at the patient and type at the same time. The nice thing about The Eye Institute is that we are very patient-centered. We have a student, sometimes a resident and a faculty member all with the same patient at times.”
“At The Eye Institute, it’s very individualized based on who the doctor is. We try to have our computers situated to the side, so the screen is facing the provider and the back of it is facing the patient,” said Dr. Parisi. “For an eye exam, there are times when you can’t get by without recording some stuff in the EMR. But our computers (in an exam room) are such that we can kind of look at the patient and type at the same time. The nice thing about The Eye Institute is that we are very patient-centered. We have a student, sometimes a resident and a faculty member all with the same patient at times.”
Dr. Parisi added that the patient-centric approach starts even before the patient steps into the exam room. A student who is assigned a patient is with that patient during the entire time they are at The Eye Institute. The student greets the patient in the waiting room and talks to them on the way to the exam room. While they’re interviewing the patients, the student is recording some data into the computer. Once a faculty member/optometrist comes into the room, the provider can dedicate his/her full attention to the patient while the student types into the EMR.
“Some practices have scribes, so our students kind of become the scribes when the doctors enter the room,” said Dr. Parisi. “Eventually we have to edit what they have written and double-check it. But while the patient is there, we expect the students to be typing in what we’re telling them. We stand in front of the patient without constantly being on the computer.”
According to Dr. Mittelman, great strides in patient-centric care has been made. Dr. Parisi agreed that the doctor-patient relationship is critical.
“You want patients to trust you and follow your recommendations at home and feel that they got the attention and were able to express what their problems were. I think that really makes a difference. The majority of people want the attention. Our patients get a lot of love and attention,” she said.